Common Medical Conditions of the Equine Hoof
If you are a horse owner, there’s a chance you will have already heard about atleast one of the medical conditions we will discuss below. The old saying “no hoof, no horse” is well worn for a reason, as proper care and maintenance of your horses feet is one of the key components to keeping them sound and comfortable. Having the appropriate team members on your horses side, as well as implementing the proper daily care, can help ensure your horses hooves remain in healthy condition. There are a few common medical conditions that can affect your horses feet, that as a horse owner are important to be aware of in order to detect early signs and understand what needs to be done.
Laminitis (Founder)
Laminitis, more commonly referred to as “founder”, is a common yet crippling disease in which there is a failure of attachment of the laminae connecting the hoof wall to the distal phalanx (coffin bone), due to inflammation in the foot. Since the laminae are responsible for suspending the distal phalanx within the hoof wall, laminar failure in combination with the downward forces of the weight of the horse can seperate the bone from the hoof wall completely. In these situations, the coffin bone may rotate within the foot, be displaced downward (“sink”) and can eventually penetrate through the sole. As you can imagine, this rotation is a very painful process and must be controlled immediately. Laminitis can affect all breeds of horses in one or all feet, but it is more commonly seen in the front feet.
While the pathogenesis of laminitis remains controversial, certain precipitating events are known to lead to to severe foot inflammation and laminitis, even so when the underlying cause is a disturbance elsewhere in the body.
These common causes include:
Grain overload or abrupt changes in diet
Sudden access to excessive amounts of lush forage before the horse’s system has had time to adapt, also known as “grass founder”
Toxins released within the horse’s system
Any illness that causes high fever or serious metabolic disturbances (ex: Potomac Horse Fever)
Severe colic
Retained placenta in mare post foaling
Excessive concusion to the feet, also known as “road founder”
Excessive weight-bearing on single leg due to injury of another leg or any other alteration of the normal gate, also known as “supporting limb laminitis”
Various primary foot diseases
Prolonged use or high doses of corticosteroids
In conjunction, certain instances increase a horse’s susceptibility to laminitis or increase the severity when it does occur, including:
Obesity
Breed - for example, heavy draft breed horses
High nutritional plane
Poor hoof care or anatomical build
Horses who have had previous episodes of laminitis
Horses with Cushings Disease or Metabolic Syndrome
Signs of an acute laminitic episode, that would warrant contacting your veterinarian, can include:
Lameness
Weight shifting
Heat in the feet and increased digital pulses (due to inflammation and blood flow to the feet)
Pain when hoof tested
Reluctance to move or “sawhorse standing” in an attempt to keep weight off the feet
Laying down
Signs of more chronic laminitis can include:
Rings visible on the outer hoof wall
Widened white line, commonly called “seedy toe,” with occurance of seromas (blood pockets) and/or abscesses
“Flat” feet or dished hooves, as the result of unequal rates of hoof growth
Diagnosis in acute lamnitis is fairly straightforward as it is based on the presence of clinical signs stated above, whereas chronis laminitis involves rotation of the distal phalanx and is diagnosed and monitored with radiographs. Treatment can differ depending on the causative agent, but in all cases of laminitis, the sooner the treatment begins and/or removal of the causative agent, the better the chance of a full recovery. Acute laminitic episodes are considered an equine emergency as rotation of the coffin bone can occur rapidly and causes permanent damage to the feet.
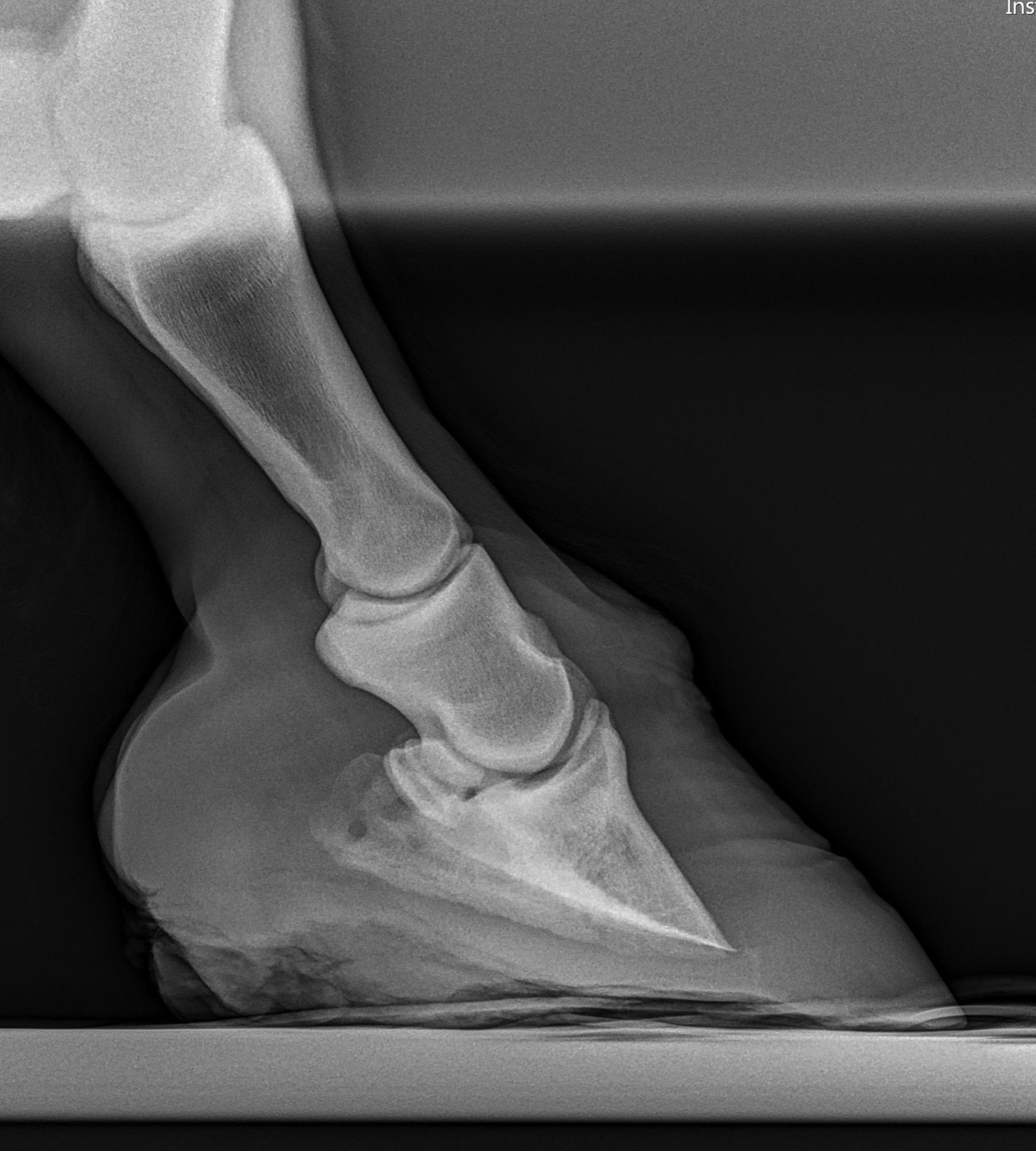
Normal foot radiograph where the distal phalanx (coffin bone) appears in line with the hoof wall, held in place by the laminae.
Radiograph following a laminitic episode that resulted in rotation of the distal phalanx (coffin bone) away from the hoof wall.
Radiograph of chronic laminitis with severe changes to the coffin bone and hoof.
Navicular Syndrome
Navicular syndrome, navicular disease and caudal heel pain/syndrome are terms often used interchangeably to reference the same condition. Navicular syndrome is a common condition for horses of all shapes and sizes that most commonly affects both front feet and causes differing severities of lameness. To better understand why it seems like one treatment works great for one horse with caudal heel pain and not for another, it is important to understand a little bit more about it. While the most common finding is abnormalities with the navicular bone, pathologic changes to the surrounding soft-tissue structures within the navicular apparatus can also contribute to navicular syndrome.
Photo credit: The Chronicle of the Horse (chronofhorse.com)
The navicular aparatus includes:
The navicular bone
The deep digital flexor tendon (DDFT) that glides down the back of the leg, over the navicular bone and attaches to the coffin bone.
The navicular bursa, that acts as a cushion in between the navicular bone and the DDFT
The collateral sesamoidean impar ligament (CSIL) that attaches the navicular bone to the coffin bone.
It is understood that navicular syndrome is caused by mechanical stress and strain due to the constant pressure between the navicular bone and DDFT, which leads to degeneration of those and other surrounding structures. Poor foot conformation, such as long toe and low heel, increases the stress and may increase development of the condition. Because of the relationship between hoof angles and the navicular apparatus structures, hoof care, as well as genetic conformation, can largely contribute to the condition. Strains and sports-related injury from highly physical disciplines requiring hard turns, fast stops lateral movements and jumping, can also increase the problem. The lameness that results is often characterized by a shortness of stride, toe-landing to take weight off the heels, reluctance to turn and pain around the center third of the frog.
Although an incurable condition, changes in the navicular apparatus doesnt necessarily mean the end of a horse’s performance career. Between nerve blocks, hoof testing, radiographs and MRI’s, the causative source of caudal heel pain can be identified and treated appropriately depending on the severity of the condition. Treatments can include and vary from:
Vet prescrived rest and rehabilitation
Corrective farrier care with therapeutic trimming and shoeing
Corticosteroid joint injections in the coffin joint and navicular bursa
Shockwave therapy
Non-steroidal anti-inflammatories
Biologics like PRP
Neurectomy (in severe cases only, as a last resort)
Hoof Abscess
It is not uncommon among horse owners to have experienced this scenario before.. your horse that was completely sound yesterday has come in from the field 3-legged lame. Although not always the case, a common cause of this scenario is what is called a hoof abscess. Bacteria enters the foot by multiple possibilities and causes an infection. Anything that weakens hoof wall or sole integrity can make it easier for bacteria to invade, from internal hoof injuries (such as bruising from stepping on a rock or sharp ice), wet conditions, poor foot balance, poor conformation or even a visit from the farrier. The mechanics caused within the hoof during laminitis, which we discussed earlier this month, can also cause the horse to be more susceptible.
The abscess starts as a localized, walled-off infection which the body fights with white blood cells and inflammatory mediators. A buildup of this infection, inflammation, and white blood cells causes an increase of pressure within the rigid hoof wall and since the pressure has no where to go, it causes a very painful result. When lameness appears and how severe the lameness becomes will vary based on the location of the abscess within the hoof and how long it takes to rupture.
Clinical signs other than lameness on the affected foot include:
Swelling
Heat
Draining tracts (pus, often gray or black in color, from the sole/coronary band indicating abscess rupture)
Increased digital pulse
Evidence of hoof injuries that allowed bacteria to enter.
Sole abscess being soaked and poulticed to keep clean and help draw the infection out.
The basic abscess treatment strategy is to open it and let it drain. Some will rupture on their own through the sole or often after traveling up the hoof to the coronary band or heel bulbs where the wall is thinner and easier to break through. Your veterinarian will use radiographs along with the previously stated clinical signs to determine the location of the abscess as to better know where to encourage the abscess rupture. In severe or chronic cases where the abscess grows deep within the hoof, radiographs can also show a deteriorating coffin bone as a result of the infection. Cleanliness is key before and after initiating drainage of the abscess, with daily soaking and poulticing required throughout the entire process. Soaking before rupture is to soften the foot and encourage drainage at the opportune location and soaking after is to ensure the foot stays clean and no bacteria re-enters, causing the process to re-occur.
Abscesses can consist of fairly simple treatment and a great prognosis, so long as they are dealt with in a timely and appropriate manner. The biggest complications come with chronic abscessation due to frequent re-occurrence, as well as over pairing of the sole without radiographic guidance causing damage of internal structures and hoof integrity.